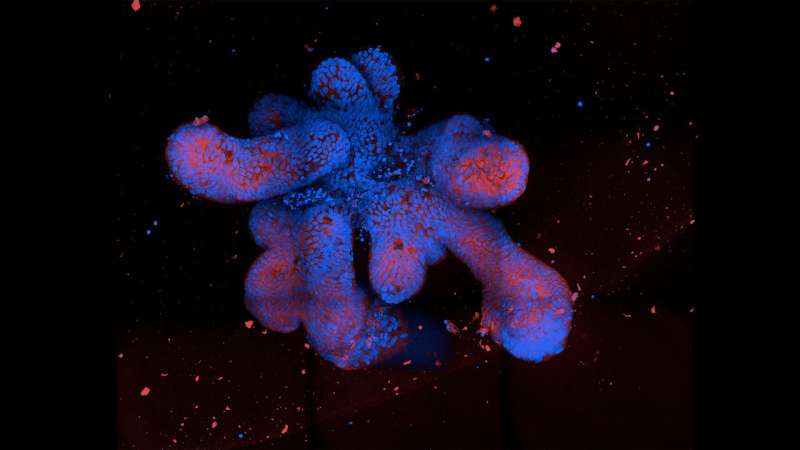
Immunofluorescence spinning disc microscopy images of organoids. Credit: Thomas Dennison/University of Cambridge
Cambridge scientists have grown ‘mini-guts’ in the lab to help understand Crohn’s disease, showing that ‘switches’ that modify DNA in gut cells play an important role in the disease and how it presents in patients.
The researchers say these mini-guts could in future be used to identify the best treatment for an individual patient, allowing for more precise and personalized treatments.
Crohn’s disease is a form of inflammatory bowel disease (IBD). It is a life-long condition characterized by inflammation of the digestive tract that affects around one in 350 people in the UK, with one in four presenting before the age of 18. Even at its mildest, it can cause symptoms that have a major impact on quality of life including stomach pain, diarrhea, weight loss and fatigue, but it can also lead to extensive surgery, inpatient admissions, exposure to toxic drugs and have a major impact on patients and their families.
While there is some evidence that an individual is at greater risk of developing the condition if a first-degree relative has Crohn’s, there has been only limited success in identifying genetic risk factors. As a result, it’s estimated that only 10% of inheritance is due to variations in our DNA.
Matthias Zilbauer, Professor of Pediatric Gastroenterology at the University of Cambridge and Cambridge University Hospitals NHS Foundation Trust (CUH), said, “The number of cases of Crohn’s disease and IBD are rising dramatically worldwide, particularly among younger children, but despite decades of research, no one knows what causes it. Part of the problem is that it’s been difficult to model the disease. We’ve had to rely mainly on studies in mice, but these are limited in what they can tell us about the disease in people.”
In research published in Gut, Professor Zilbauer and colleagues used cells from inflamed guts, donated by 160 patients, mainly patients and adolescents, at CUH to grow more than 300 mini-guts—known as organoids—in the lab to help them better understand the condition. Samples were donated by patients with Crohn’s disease and ulcerative colitis, as well as by patients unaffected by IBD.
“The organoids that we’ve generated are primarily from children and adolescents,” said Professor Zilbauer. “They’ve essentially given us pieces of their bowel to help with our research. Crohn’s can be a severe condition to have to deal with at any age, but without our volunteers’ bravery and support, we would not be able to make such discoveries as this.”
Organoids are 3D cell cultures that mimic key functions of a particular organ, in this case the epithelium—the lining of the gut. The researchers grew them from specific cells, known as stem cells, taken from the gut. Stem cells live forever in the gut, constantly dividing and allowing the gut epithelium to regenerate.
Using these organoids, they showed that the epithelia in the guts of Crohn’s disease patients have different ‘epigenetic’ patterns on their DNA compared to those from healthy controls. Epigenetics is where our DNA is modified by ‘switches’ attached to our DNA that turn genes on and off—or turn their activity up or down—leaving the DNA itself intact, but changing the way a cell functions.
Professor Zilbauer, a researcher at the Stem Cell Institute at the University of Cambridge, said, “What we saw was that not only were the epigenetic changes different in Crohn’s disease, but there was a correlation between these changes and the severity of the disease. Every patient’s disease course is different, and these changes help explain why—not every organoid had the same epigenetic changes.”
The researchers say the organoids could be used to develop and test new treatments, to see how effective they are on the lining of the gut in Crohn’s disease. It also opens up the possibility of tailoring treatments to individual patients.
Co-author Dr. Robert Heuschkel, Consultant Pediatric Gastroenterologist at CUH and Lead of the Pediatric IBD Service, said, “At the moment, we have no way of knowing which treatment will work best for a patient. Even those treatments we currently have only work in around half of our patients and become less effective over time. It’s a huge problem.
“In future, you could imagine taking cells from a particular patient, growing their organoid, testing different drugs on the organoid, and saying, ‘OK, this is the drug that works for this person.'”
The research highlighted a specific pathway implicated in Crohn’s, known as major histocompatibility complex (MHC)-I. This pathway allows immune cells to recognize antigens—that is, a toxin or other foreign substance that induces an immune response in the body, and which could include molecules in our food, or our gut microbiota.
The team showed that the cells forming the inner lining of the gut in Crohn’s disease patients have an increased activity of MHC-I, which can lead to inflammation in specific parts of the gut.
“This is the first time where anyone has been able to show that stable epigenetic changes can explain what is wrong in the gut epithelium in patients with Crohn’s disease,” said Professor Zilbauer.
The epigenetic modifications were found to be very stable, which may explain why even after treatment, when a patient appears to be healed, their inflammation can return after several months—the drugs are treating the symptoms, not the underlying cause.
Epigenetic changes are programmed into our cells very early on during the development of the baby in the womb. They are influenced by environmental factors, which may include exposure to infections or antibiotics—or even lack of exposure to infection, the so-called ‘hygiene hypothesis’ that says we are not exposed to sufficient microbes for our immune systems to properly develop.
The researchers say this may offer one possible explanation for how the epigenetic changes that lead to Crohn’s disease occur in the first place.
The research was largely supported by the Medical Research Council. It was also supported through collaboration with the Milner Therapeutics Institute, University of Cambridge.
Cambridge Enterprise is working with Professor Zilbauer and team and has recently filed a patent for this technology. They are seeking commercial partners to help with the development of this opportunity.
More information:
Dennison, T et al. Patient-derived organoid biobank identifies epigenetic dysregulation of intestinal epithelial MHC-I as a novel mechanism in severe Crohn’s disease, Gut (2024). DOI: 10.1136/gutjnl-2024-332043
Citation:
Lab-grown ‘mini-guts’ could help in development of new and more personalized treatments for Crohn’s disease (2024, June 10)
retrieved 11 June 2024
from https://medicalxpress.com/news/2024-06-lab-grown-mini-guts-personalized.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
>>> Read full article>>>
Copyright for syndicated content belongs to the linked Source : Medical Xpress – https://medicalxpress.com/news/2024-06-lab-grown-mini-guts-personalized.html










