Can Liver Damage from Alcohol Be Reversed? Doctor Reveals Truth
As alcohol consumption continues to pose significant health risks, the concern about its impact on the liver remains a pressing issue for millions globally. With staggering statistics indicating that liver-related diseases are on the rise, the questions surrounding the potential for reversing alcohol-induced liver damage have garnered widespread attention. In this comprehensive article, we delve into the insights of medical experts who shed light on the complexities of liver health, exploring the extent to which the liver can heal itself after years of alcohol abuse. From understanding the stages of liver damage to examining the latest treatment options and lifestyle changes, we aim to provide a nuanced perspective on the path towards recovery. Join us as we uncover the truths behind liver health and the critical steps individuals can take to reclaim their well-being.
Assessing the Impact of Alcohol on Liver Health and the Potential for Recovery
The relationship between alcohol consumption and liver health is complex, with various factors determining the extent of damage and recovery potential. Chronic alcohol use can lead to a spectrum of liver conditions, such as fatty liver disease, alcoholic hepatitis, and cirrhosis. It’s essential to recognize that the degree of liver damage greatly influences recovery outcomes. While early-stage fatty liver disease may show signs of reversal upon cessation of alcohol use, more advanced conditions like cirrhosis could result in permanent damage. Key factors affecting recovery include:
- Duration of alcohol use: Long-term consumption increases the risk of irreversible damage.
- Presence of liver disease: Pre-existing liver conditions can complicate recovery.
- Overall health: Co-existing health issues, such as obesity and diabetes, can hinder recovery.
- Support systems: Access to medical treatments and rehabilitation services greatly enhances recovery chances.
Research indicates that the liver has a remarkable ability to regenerate, yet the timeline and extent of recovery vary significantly. A study conducted by the American Journal of Gastroenterology highlighted that individuals who quit alcohol for at least six months recorded substantial improvements in liver function test results. To illustrate the potential for recovery, the following table outlines the stages of liver disease and corresponding recovery prospects:
| Stage of Liver Disease | Possible Recovery Actions | Recovery Potential |
|---|---|---|
| Fatty Liver | Alcohol cessation, diet, exercise | High |
| Alcoholic Hepatitis | Medical intervention, abstinence | Moderate |
| Cirrhosis | Abstinence, lifestyle changes, medications | Low to Moderate |
Understanding the Stages of Alcohol-Related Liver Damage and Their Reversibility
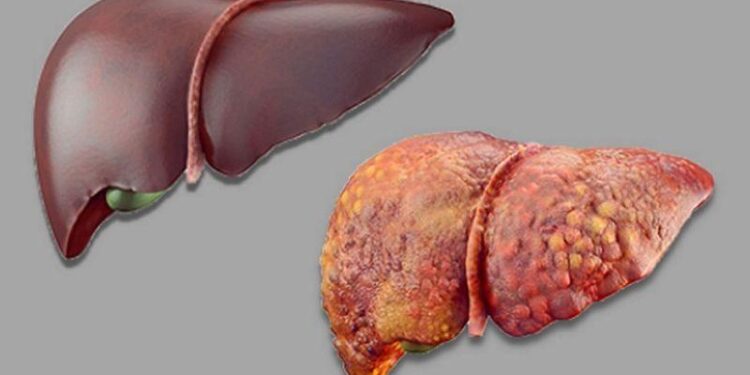
Alcohol-related liver damage progresses through distinct stages, each characterized by specific changes in liver tissue and function. The initial stage, known as fatty liver (steatosis), occurs when excess fat begins to accumulate in liver cells, often without causing any significant symptoms. If alcohol consumption continues, this can advance to alcoholic hepatitis, where inflammation sets in, potentially leading to symptoms such as jaundice, abdominal pain, and fever. The final stage, cirrhosis, involves irreversible scarring of the liver, severely impairing its ability to function. Understanding these stages is crucial as the earlier they are identified, the more likely it is that damage can be reversed with lifestyle modifications and abstinence from alcohol.
While the liver has a remarkable capacity for regeneration, the reversibility of damage largely hinges on the stage at which intervention occurs. Research indicates that fatty liver can often be reversed with relatively simple lifestyle changes, while alcoholic hepatitis may lead to significant recovery with early medical intervention. However, cirrhosis presents a more complex challenge as the damage at this stage is frequently irreversible. It is essential for individuals grappling with alcohol use to be aware of the potential for recovery and the importance of seeking medical guidance promptly to mitigate further damage. Regular monitoring and lifestyle adjustments, such as adopting a balanced diet, increasing physical activity, and avoiding all alcohol, can dramatically improve outcomes in earlier stages.
| Stage of Damage | Description | Reversibility |
|---|---|---|
| Fatty Liver | Accumulation of fat in liver cells | High |
| Alcoholic Hepatitis | Inflammation of the liver | Moderate |
| Cirrhosis | Severe scarring and liver function impairment | Low |
Expert Recommendations for Reversing Liver Damage Through Lifestyle Changes and Medical Intervention
To combat liver damage and promote healing, experts strongly recommend a combination of lifestyle modifications and medical interventions. Adopting healthier eating habits is essential; individuals should focus on a diet rich in antioxidants, healthy fats, and fiber. Some vital dietary tips include:
- Increase intake of fruits and vegetables: Foods high in vitamins E and C can help protect liver cells.
- Incorporate lean proteins: Skinless poultry, fish, and plant-based proteins can support liver regeneration.
- Stay hydrated: Drinking adequate water helps flush toxins from the liver.
In addition to dietary changes, regular exercise plays a significant role in liver health. Engaging in moderate physical activity helps maintain a healthy weight and can reduce liver fat. Furthermore, for those struggling with severe liver damage, seeking medical intervention is crucial. Healthcare professionals may recommend:
- Regular screenings: Monitoring liver enzymes can help assess damage progress.
- Medication: Certain drugs may be prescribed to assist with detoxification and repair.
- Consultation with specialists: Gastroenterologists can provide tailored treatment plans based on individual needs.
To Conclude
while the path to recovery from alcohol-related liver damage is complex, expert insights reveal that with early intervention and lifestyle changes, significant healing is indeed possible. As highlighted by medical professionals, the liver possesses a remarkable capacity for regeneration, but this requires a commitment to abstinence from alcohol and a healthy lifestyle. Readers are encouraged to consult healthcare providers for personalized advice, as individual conditions may vary. As awareness grows about the risks of alcohol consumption, it is vital to prioritize liver health and seek help when needed. The journey to recovery is not only a matter of personal health but also a broader societal challenge that calls for understanding and support.