The National Institutes of Health (NIH) has spotlighted the critical role of mitochondria in maintaining human health, emphasizing new insights into how these cellular powerhouses influence a range of diseases. As research advances, understanding mitochondrial function and dysfunction is proving essential in addressing conditions from metabolic disorders to neurodegenerative diseases. This article explores the latest findings from the NIH on mitochondria, highlighting their significance in health and potential avenues for therapeutic intervention.
Mitochondria’s Role in Energy Production and Chronic Disease Prevention
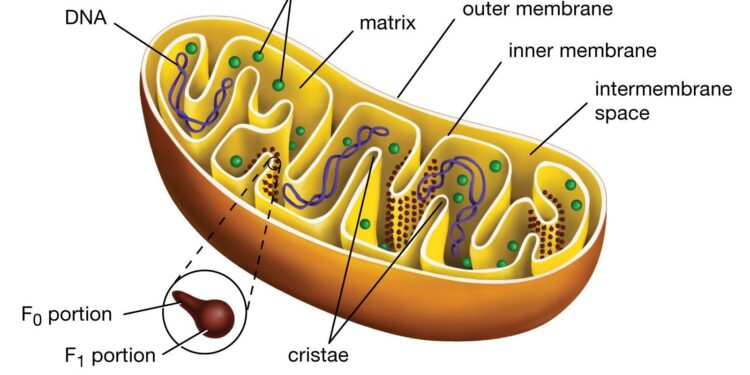
Mitochondria are often dubbed the “powerhouses” of our cells, and for good reason. These tiny organelles generate adenosine triphosphate (ATP), the main energy currency that fuels nearly every cellular function. Without efficient mitochondrial activity, tissues and organs struggle to perform at optimal levels, impacting overall vitality and health. Recent research underscores how mitochondrial efficiency is not only vital for energy metabolism but also plays a critical role in modulating oxidative stress and inflammation, two key drivers of chronic diseases.
Emerging evidence links mitochondrial dysfunction to a spectrum of chronic health conditions, including diabetes, cardiovascular disorders, and neurodegenerative diseases. Strategies targeting mitochondrial health could revolutionize prevention and treatment protocols. Key factors that support robust mitochondrial function include:
- Regular physical activity to stimulate mitochondrial biogenesis
- Balanced nutrition rich in antioxidants and micronutrients
- Stress management to reduce oxidative damage
- Quality sleep which is essential for mitochondrial repair
| Factor | Impact on Mitochondria | Chronic Disease Link |
|---|---|---|
| Exercise | Increases mitochondrial number and function | Reduces risk of diabetes and heart disease |
| Antioxidants | Neutralize harmful free radicals | Prevents neurodegeneration |
| Sleep | Facilitates cellular repair | Supports metabolic health |
How Mitochondrial Dysfunction Impacts Aging and Metabolic Health
Mitochondrial dysfunction is increasingly recognized as a key driver of the aging process and the development of metabolic disorders. As the powerhouses of the cell, mitochondria produce the energy necessary for cellular function through oxidative phosphorylation. However, when mitochondria fail to operate efficiently, cells experience energy deficits, increased oxidative stress, and impaired metabolic signaling. This cascade contributes to the decline in tissue function seen with age, impacting vital organs such as the brain, muscles, and liver. Emerging research highlights how damaged mitochondria also secrete harmful byproducts that exacerbate inflammation, accelerating age-related diseases like type 2 diabetes, cardiovascular conditions, and neurodegeneration.
Several hallmark effects of mitochondrial dysfunction on metabolic health include:
- Reduced ATP production: Limits energy availability for cellular repairs and maintenance.
- Excess reactive oxygen species (ROS): Promotes oxidative damage to DNA, proteins, and lipids.
- Disrupted metabolic homeostasis: Impairs regulation of glucose and lipid metabolism, fostering insulin resistance.
- Alterations in mitochondrial dynamics: Reduced biogenesis and impaired mitophagy compromise mitochondrial quality control.
| Impact | Consequence | Potential Outcome |
|---|---|---|
| Energy Deficit | Cellular dysfunction | Muscle weakness, fatigue |
| Oxidative Stress | Macromolecular damage | Chronic inflammation, aging |
| Metabolic Imbalance | Insulin resistance | Type 2 diabetes |
NIH Guidelines for Supporting Mitochondrial Health Through Diet and Lifestyle
The National Institutes of Health emphasize a holistic approach to maintaining mitochondrial function, recognizing its critical role in energy production and overall cellular health. Their recommendations highlight a balanced diet rich in antioxidants, essential nutrients, and healthy fats. Key dietary elements include foods high in Coenzyme Q10, B vitamins, and polyphenols, which help combat oxidative stress and promote efficient mitochondrial energy pathways. Additionally, limiting excessive processed sugars and saturated fats is advised to reduce mitochondrial dysfunction linked to metabolic disorders.
Lifestyle factors are equally pivotal in supporting mitochondrial vitality. The NIH advocates for regular physical activity, stress management, and adequate sleep to optimize mitochondrial biogenesis and function. Below is a quick overview of their suggested practices:
- Engage in moderate-intensity aerobic exercise for at least 150 minutes weekly
- Incorporate mindfulness techniques such as meditation or yoga to reduce oxidative stress
- Prioritize 7-9 hours of restorative sleep per night to facilitate cellular repair mechanisms
| Factor | NIH Recommendation | Impact on Mitochondria |
|---|---|---|
| Diet | Antioxidant-rich foods & balanced macro intake | Reduces oxidative damage, supports energy production |
| Exercise | Regular aerobic and resistance training | Promotes mitochondrial biogenesis |
| Sleep | 7-9 hours nightly | Enhances mitochondrial repair and recovery |
| Stress Management | Mindfulness and relaxation techniques | Decreases mitochondrial dysfunction linked to stress |
Wrapping Up
As research from the National Institutes of Health continues to shed light on the critical role of mitochondria in overall health, it becomes increasingly clear that these cellular powerhouses are integral to understanding and potentially treating a wide range of diseases. Ongoing studies promise to unravel new therapeutic avenues, emphasizing the importance of mitochondria in medical science. Staying informed on these developments is essential for both healthcare professionals and the public as we move towards more targeted and effective health interventions.