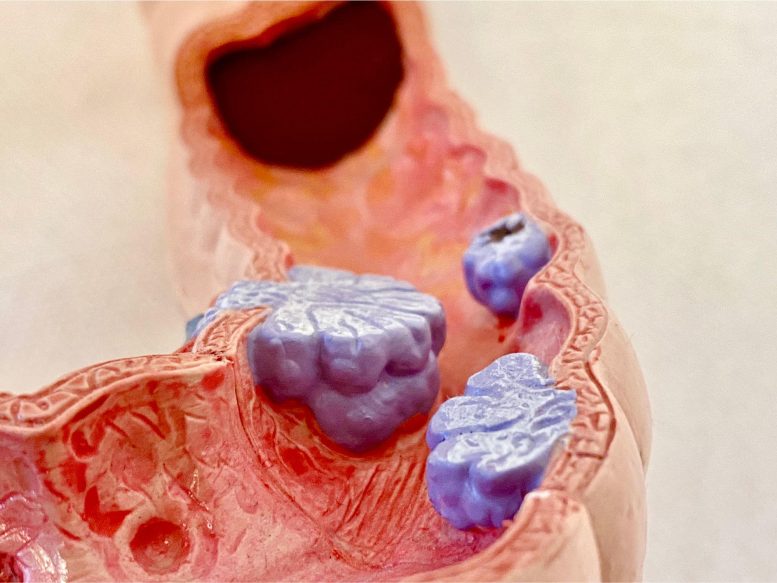
Colon polyps are abnormal growths that develop in the lining of the colon or rectum. While most polyps are benign, some can become cancerous over time.
Grasping the connection between the gut microbiome and the polyp growth paves the way for potential diagnostic procedures and treatments.
Researchers from Mass General Brigham have recently published a study in the journal Cell Host & Microbe that establishes a connection between specific gut bacteria and the formation of precancerous polyps in the colon.
“Researchers have done a lot of work to understand the relationship between the gut microbiome and cancer. But this new study is about understanding the microbiome’s influence on precancerous polyps,” said co-corresponding author Daniel C. Chung, MD, medical co-director of the Center for Cancer Risk Assessment at the Mass General Cancer Center and a faculty member of the Gastroenterology Division. “Through the microbiome, we potentially have an opportunity to intervene and prevent colorectal cancer from forming.”
Colorectal cancer, the second most deadly type of cancer in the U.S., is seeing an increase in incidence among younger adults. Almost all colorectal cancers originate from a precancerous polyp. Therefore, one of the most effective strategies to decrease colorectal cancer rates is to halt the progression at the polyp stage.
There’s more than one way for a polyp to develop. The two main types of polyps are tubular adenomas and sessile serrated polyps. Risk factors for colorectal cancer and polyps include lifestyle factors like being overweight or obese, low physical activity levels, a diet high in red and processed meats, smoking, and alcohol use. These factors also influence the bacteria that live in our intestines, collectively known as the gut microbiome.
Researchers think these environmental influences could promote polyp growth in one of two ways. Either they change the gut microbiome directly in a way that encourages polyp growth, or they promote polyp growth which in turn influences the gut microbiome by directly affecting the cells lining the intestines.
Earlier, smaller studies trying to link the gut microbiome to polyps have not found a consistent pattern, though they didn’t look at these two types of polyps specifically.
To study the gut microbiome’s link to colon polyps, the researchers took data from 1,200 people getting routine screening colonoscopies. They gathered information on their health, diet, medications, and lifestyle, as well as analyzed stool samples to determine the bacterial makeup of their gut microbiome. The new research is the biggest study from an extensive collaborative research program, the GI Disease and Endoscopy Registry (GIDER) at Massachusetts General Hospital, allowing these researchers to understand gastrointestinal diseases in greater depth than ever. This registry remains active and ongoing data collection will enable longitudinal follow-up.
The new study is the largest of its kind and analyzed the differences in the gut microbial signature of people without colon polyps, with tubular adenomas, or with sessile serrated adenomas. They also correlated this data with the patient’s health and family histories.
Bacterial signatures clustered into three groups based on the type and presence of polyps in the colon. Nineteen bacterial DOI: 10.1016/j.chom.2023.04.007
The study was funded in part by the Center for Microbiome Informatics and Therapeutics at