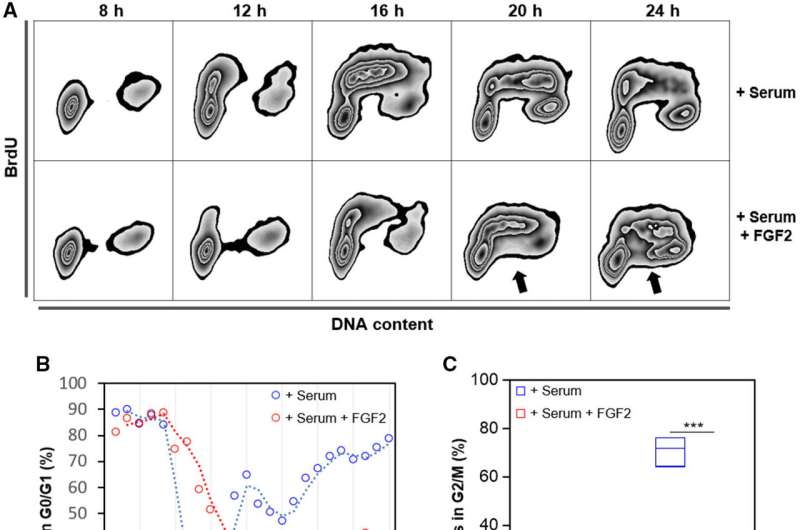
FGF2 impairs cell cycle progression in K-Ras-driven cancer cells. Serum-starved Y1D1 cells were stimulated by 10% serum with or without 10 ng·mL−1 FGF2 to re-entry the cell cycle. Cells were subjected to a BrdU pulse 30 min before sample collection (every two hours). Credit: Cancer Discovery (2024). DOI: 10.1158/2159-8290.CD-23-0216
A combination of two drugs was capable of suppressing tumors in a non-conventional manner. Instead of inhibiting tumor cell division, as the most widely used medications do, the strategy consisted of hyperactivating oncogenic signaling by these cells to the point where they became stressed. The other drug then attacked the stressed cells. The approach will be tested in colorectal cancer patients in the Netherlands later this year.
The study is published in Cancer Discovery. The first author is Matheus Henrique Dias, a Brazilian who is currently a senior postdoctoral fellow at the Netherlands Cancer Institute (NKI).
The idea began to develop while Dias was doing postdoctoral research at Butantan Institute in São Paulo, Brazil, and an internship at the University of Liverpool in the United Kingdom. The project was conducted under the aegis of the Center for Research on Toxins, Immune Response and Cell Signaling (CeTICS), a Research, Innovation and Dissemination Center (RIDC).
“Back then, we discovered that a gene known as fibroblast growth factor 2 [FGF2] inhibited multiplication of tumor cells instead of stimulating it, as it did in the case of healthy cells. This was a surprise since it was the opposite of what should happen,” Dias told.
At the time, a study on the role of FGF2 was published in the journal Molecular Oncology.
In this latest paper, the researchers show that cancer cells do not multiply less because they are inhibited directly by a drug, as in the case of conventional chemotherapy. On the contrary, one of the drugs used in this strategy triggers hyperactivation of tumor cell signaling, stressing the cells and making them sensitive to specific drugs for cells in this state.
“As a rough analogy, imagine you’re in a very fast car and instead of braking to stop it you step hard on the accelerator until the engine overheats. And you turn off the cooling system just when the engine gets really hot,” Dias said.
Dual attack
Another co-author of the study, Marcelo Santos da Silva, a professor at the University of São Paulo’s Institute of Chemistry (IQ-USP), was doing postdoctoral research at Butantan Institute at the same time as Dias and developed an assay to quantify stress in tumor cells.
“When tumor cells are hyperactivated, they replicate DNA even faster than usual, but their DNA is damaged because they aren’t equipped to handle such rapid replication. This is known as replicative stress,” he said.
Observing that hyperactivation of FGF2 stressed the cells sufficiently to inhibit their multiplication, Dias decided to look for a molecule that could induce this process. The most promising candidate was LB-100, currently being tested in clinical trials to confirm that it makes lung tumors sensitive to chemotherapy drugs.
To attack cells stressed by the action of LB-100, the researchers chose inhibitors of the protein WEE1, which is responsible precisely for repairing tumor DNA damage. When this mechanism is not working, tumor cells divide before completing DNA replication and die as a result.
“The most interesting part is that cancer cells deactivate oncogenic pathways in order to survive this approach and then behave like healthy cells,” Dias said.
The trials involved colorectal tumor cells taken from human biopsies and implanted in mice. Treatment with the two drugs inhibited tumor growth in the animals.
In light of their success in colorectal cancer models, the researchers went on to test the combination on pancreatic adenocarcinoma and cholangiocarcinoma (bile duct) cell lines. These are rarer and more aggressive types of cancer with few treatment options. The results were equally promising.
“This is a growing research field, with large corporations investing in signaling activators and startups being founded to develop this kind of drug. In the years ahead, some will be on the market as options for cancer treatment. We hope one of them is ours,” Dias said.
At USP, Silva plans to apply the principle used in the potential cancer treatment to eliminate parasites that cause neglected tropical diseases. The protozoans that cause Chagas disease and others that cause leishmaniasis behave similarly to cancer cells inasmuch as they replicate very quickly inside host cells.
“I propose to use a drug that stimulates the proliferation signaling pathway in parasites sufficiently to cause the same kind of DNA damage, and then administer another drug to repair the DNA. This should eliminate the parasite without harming host cells,” Silva said.
More information:
Matheus Henrique Dias et al, Paradoxical Activation of Oncogenic Signaling as a Cancer Treatment Strategy, Cancer Discovery (2024). DOI: 10.1158/2159-8290.CD-23-0216
Citation:
Combination drug strategy produces promising results by hyperactivating oncogenic signaling (2024, July 26)
retrieved 26 July 2024
from https://medicalxpress.com/news/2024-07-combination-drug-strategy-results-hyperactivating.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
>>> Read full article>>>
Copyright for syndicated content belongs to the linked Source : Medical Xpress – https://medicalxpress.com/news/2024-07-combination-drug-strategy-results-hyperactivating.html










