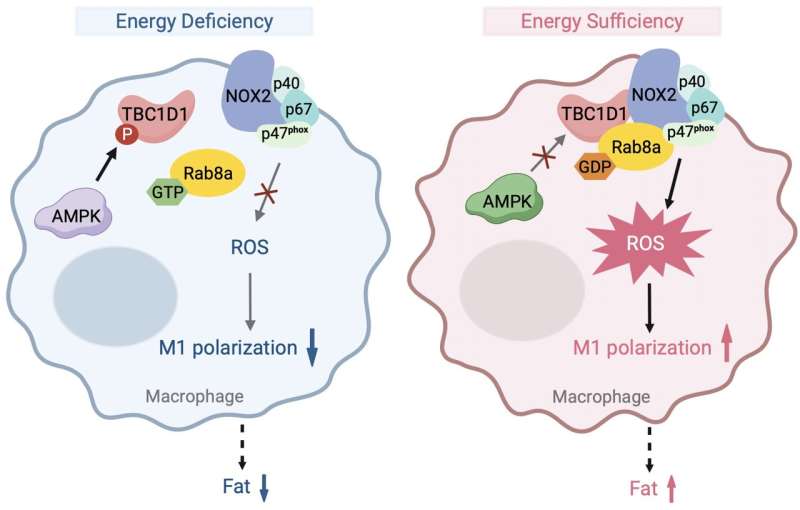
A diagrammatic illustration represents the proposed model. The energy sensor AMPK becomes less active under energy overload conditions, which leads to hypophosphorylation of TBC1D1. Hypophosphorylated TBC1D1 is more active and converts Rab8a to its GDP-bound form. TBC1D1 and GDP-bound Rab8a interacts with NOX2, and enhances its enzymatic activity to generate ROS, which promotes M1 polarization in macrophages and consequent development of obesity. Credit: Qi Wang.
Metabolic and immune pathways are highly regulated and interwoven by multiple mechanisms to govern metabolic health. Dysregulation of these pathways underlies the development of metabolic diseases such as obesity and type 2 diabetes (T2D), which have become prevalent worldwide in recent years.
Thus far, the molecular mechanisms for interaction of metabolic and immune pathways are not fully understood. Shuai Chen and Hong-Yu Wang, together with lab members Qi Wang and Ping Rong, sought to determine the mechanisms for the interaction. Their work is published in the journal Science China Life Sciences.
As an important energy sensor, AMP-activated protein kinase (AMPK) can respond to the energy status to maintain metabolic homeostasis. Energy status is associated with the production of reactive oxygen species (ROS) in macrophages, which are elevated in obesity. However, it is not clear how ROS production is upregulated in the presence of sufficient energy in macrophages.
Rab-GTPase activating protein (RabGAP) TBC1D1 is a substrate for AMPK. Previous studies have shown that AMPK kinase can regulate the phosphorylation of serine-231 on TBC1D1 protein, thereby altering its GAP activity. A TBC1D1S231A mutation can elicit a sham energy-sufficient signal. The research group has shown that the TBC1D1S231A mutation results in obesity, hyperglycemia, insulin resistance, hyperlipidemia, nonalcoholic fatty liver and other metabolic diseases in mice.
Here, the team found that ROS levels in both bone marrow derived macrophages (BMDMs) and adipose tissue macrophages of TBC1D1S231A mice were significantly higher than those of wild-type mice. Moreover, macrophages from TBC1D1S231A mice exhibited M1-type (classically activated) macrophage polarization.
In contrast, ROS levels were significantly reduced in both bone marrow macrophages and adipose tissue macrophages in TBC1D1 knockout (KO) mice that were leaner than WT controls. Macrophages from TBC1D1-KO mice displayed M2-type (alternatively-activated) macrophage polarization.
To establish a role of TBC1D1 in macrophages on obesity, the team conducted a bone marrow transfer experiment. Bone marrow from TBC1D1S231A mice was transplanted into wild-type mice, and the recipient mice developed obesity. These data suggest that TBC1D1 is a key regulator of reactive oxygen species production and inflammatory states in macrophages to promote obesity.
The team then investigated how TBC1D1 regulates ROS production in macrophages. They found that TBC1D1 regulated a small G protein Rab8a to govern ROS production in macrophages. The GDP-bound form of Rab8a increased ROS production in cells. Bone marrow-specific Rab8a knockout mice had lighter body weight with reduced M1 polarization. Mechanistically, GDP-bound Rab8a interacted with NADPH oxidase NOX2 in macrophages to promote ROS production. These data suggest that the TBC1D1S231A mutation may augment ROS production by increasing GDP-bound Rab8a, and consequently elicit inflammation.
To further verify the role of ROS in the progression of obesity in TBC1D1S231A mice, the team utilized a ROS scavenger TtSOD that entered the body through the intestine and targeted macrophages in adipose tissue specifically. TtSOD treatment alleviated the obesity and inflammation in adipose tissue of TBC1D1S231A mice, and also ameliorated metabolic diseases such as hyperglycemia, hyperinsulinemia, hypercholesterolemia and insulin resistance.
Moreover, TtSOD treatment also alleviated diet-induced obesity and the associated metabolic disorders such as hyperglycemia, hypercholesterolemia and insulin resistance.
In summary, this study elucidates a novel regulatory mechanism governing ROS production in macrophages in response to energy overload, in which TBC1D1 and its downstream target Rab8a form an energy-responsive complex with NOX2 to control ROS production and consequent inflammation. These findings have implications for drug discovery to combat obesity.
More information:
Qi Wang et al, TBC1D1 is an energy-responsive polarization regulator of macrophages via governing ROS production in obesity, Science China Life Sciences (2024). DOI: 10.1007/s11427-024-2628-1
Citation:
New insights into metabolic and immune pathway interactions in obesity (2024, July 5)
retrieved 6 July 2024
from https://medicalxpress.com/news/2024-07-insights-metabolic-immune-pathway-interactions.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
>>> Read full article>>>
Copyright for syndicated content belongs to the linked Source : Medical Xpress – https://medicalxpress.com/news/2024-07-insights-metabolic-immune-pathway-interactions.html
