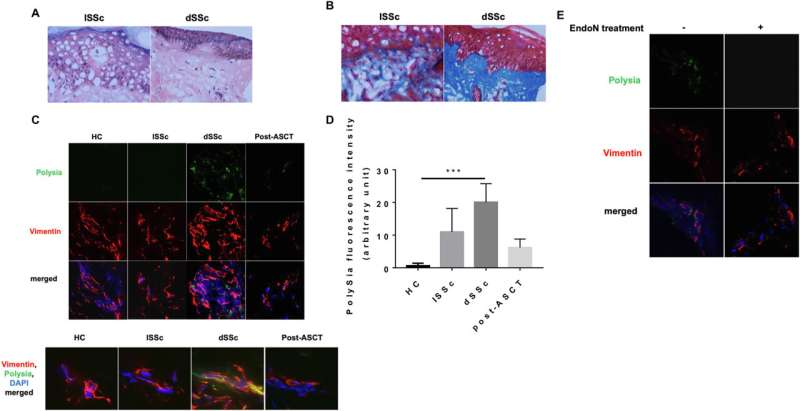
PolySia expression is highest in the fibrotic skin of dSSc patients. Skin biopsy sections from the different groups were used for our experiments. Credit: Journal of Autoimmunity (2023). DOI: 10.1016/j.jaut.2023.103110
A cross-disciplinary University of Alberta research team has uncovered a biological marker for scleroderma that can predict which patients will develop severe disease and could also lead to new treatments.
Scleroderma is a rare condition that affects about 17,000 people in Canada. An overproduction of collagen leads to a hardening of the skin, and in severe cases, blood vessels and internal organs are also affected. Approximately 40% of patients die within five years of diagnosis.
Medication, diet and exercise may slow progression and ease symptoms, but there is no cure, and until now there has been no way to predict who will develop the most severe form of the disease.
In recently published research, the team found that polysialic acid is elevated in both the skin and blood of patients with systemic sclerosis and correlates with the level of fibrosis. Polysialic acid is a glycan, or sugar modification, on the surface of cells in the immune, reproductive and nervous systems, and is known to be associated with aggressive cancer cells as well. The research was published in Journal of Autoimmunity.
“Scleroderma is a terrible disease that starts with debilitating fatigue and then leads to systemic scarring. Imagine basically feeling trapped in your own body,” says co-principal investigator Mo Osman, rheumatologist and immunologist and associate professor in the Faculty of Medicine & Dentistry.
“It’s key to identify those whose disease will progress because we want to be able to treat them early to minimize damage,” Osman says.
Co-principal investigator Lisa Willis, assistant professor in the Faculty of Science and an expert on glycans, developed the blood test for polysialic acid in her lab.
“What you need for a biomarker is something that can be used cheaply in a clinic,” Willis says. “We developed our test to be able to look for our molecule from the vial of blood that was already taken from a patient at diagnosis.”
Although scleroderma is generally considered an inflammatory autoimmune disorder, it often does not respond to treatments that suppress the immune system. About three patients a year in Edmonton receive a stem cell transplant to replace bone marrow that’s not working properly. The treatment costs about $80,000 per patient and requires patients to go to Calgary for three months, Osman says.
The researchers reported that patients who had received a bone marrow transplant showed reduced levels of polysialic acid, an indicator that changes in the glycan are directly related to the disease process.
For the study, blood and tissue samples were taken from five healthy control patients, five patients with skin fibrosis only, 11 patients with more severe fibrosis and four patients who had received transplants.
Willis and Osman had not worked together before, but both were struck by previously observed similarities between scleroderma and cancer.
“This is the most exciting type of science,” says Osman. “We thought, “It’s very interesting that immune cells in scleroderma behave very similarly to immune cells in cancer, so what’s going on? Maybe there’s a connection.'”
Willis says they postulate that the glycan is interfering with the body’s ability to deal with scarring.
“Sugars form a really thick layer on the outside of a cell that is responsible for mediating the interactions between the cell and its environment. The sugars are what the immune system uses to say, ‘OK, this is self, I don’t want to attack this’ or, ‘This is foreign, I should deal with it.’
“Normally, the immune system should recognize those pathogenic scleroderma cells, but the scleroderma cells make the glycan so they can grow without being killed.”
Willis and Osman will continue testing the biomarker as a diagnostic tool by looking at skin and blood samples from a broader cross-section of patients from across Canada and other parts of the world.
They are also working to pinpoint the mechanism involved.
“We’ve developed some more technology that allows us to find the proteins this glycan is attached to, so we can start to figure out how it is actually causing these changes,” explains Willis. “That might hint as to how we could potentially develop new therapeutics to intervene.”
Osman hopes the shared work will lead to a brand new avenue of treatment for scleroderma.
“This is a paradigm shift—a potentially very important different way of looking at how to manipulate immune responses. As an immunologist, that’s very exciting.”
Both researchers credit their trainees for conducting their experiments in close collaboration, including holding joint lab meetings.
“My students will develop a reagent, then walk across campus to give stuff to Mo’s lab, and vice versa,” Willis says.
More information:
Lamia Khan et al, The cancer-associated glycan polysialic acid is dysregulated in systemic sclerosis and is associated with fibrosis, Journal of Autoimmunity (2023). DOI: 10.1016/j.jaut.2023.103110
Citation:
Study uncovers new biological marker for scleroderma (2024, January 9)
retrieved 9 January 2024
from https://medicalxpress.com/news/2024-01-uncovers-biological-marker-scleroderma.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
>>> Read full article>>>
Copyright for syndicated content belongs to the linked Source : Medical Xpress – https://medicalxpress.com/news/2024-01-uncovers-biological-marker-scleroderma.html
