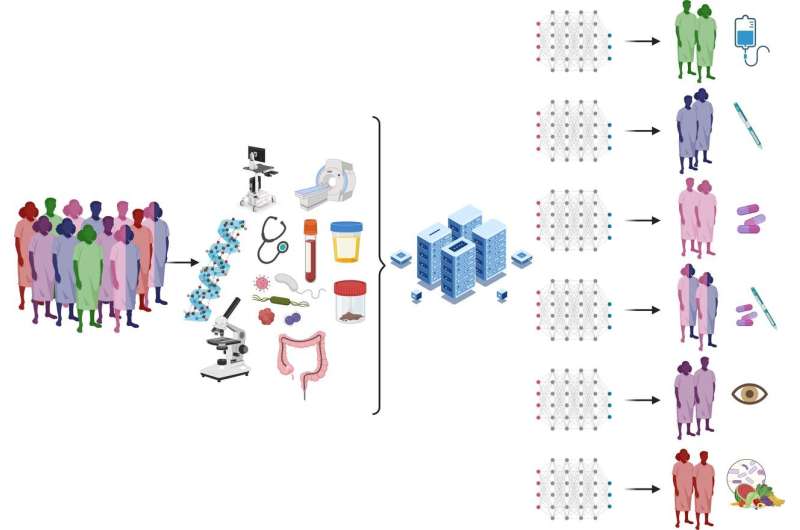
In this approach, patients are assessed using a combination of clinical and molecular profiling, incorporating genetic, immunological and microbial evaluation. Complex raw data are interpreted by omics-based network medicine, allowing accurate molecular profiling of patient groups and informed selection of a therapeutic agent, combination therapy, observation or novel dietary or microbial interventions. Created with BioRender.com. IBD, inflammatory bowel disease. Credit: Little RD, Jayawardana T, Koentgen S, et al.
The prevalence of inflammatory bowel disease (IBD), encompassing ulcerative colitis (UC) and Crohn’s disease (CD), is rapidly increasing worldwide, affecting an estimated 6.8 million people. This surge brings significant economic burdens, with annual health care costs exceeding $12,000 and $7,000 for CD and UC patients, respectively. Tailored drug selection based on individual factors can potentially reduce these costs and improve patient outcomes.
Factors associated with a Western lifestyle, such as urbanization, high animal protein intake, ultra-processed foods, and reduced fiber consumption are linked to IBD onset. Gut microbial diversity also plays a key role, with rural communities exhibiting greater microbial richness than urban populations. Understanding these environmental and microbial influences is crucial for developing preventive strategies.
Despite significant scientific advancements, the exact causes of UC and CD remain elusive. A complex interplay of genetics, immune dysregulation, gut microbiota alterations, and environmental factors contributes to disease development. Current immunosuppressive treatment options require more personalized approaches.
Major community and species-specific alterations in gut microbiota and metabolites associated with active inflammatory bowel disease (right) relative to healthy bowel (left). Created with BioRender.com. SCFA, short-chain fatty acid. Credit: Little RD, Jayawardana T, Koentgen S, et al.
The field of precision medicine offers hope for personalized IBD treatment. It can potentially predict treatment response and optimize therapy selection by analyzing individual genetic, immunological, and microbial profiles. This “multiomics” approach, coupled with machine learning, holds the key to unlocking new therapeutic targets and improving patient outcomes.
A new review appearing in eGastroenterology dives deeper into IBD’s genetic, immunological, and microbial drivers, highlighting potential predictive markers of treatment response. The researchers explore the principles of machine-learning-powered bioinformatics and collaborative research, paving the way for future precision medicine strategies in IBD. By embracing personalized approaches, they believe we can unlock a brighter future for patients living with this chronic condition.
More information:
Robert D Little et al, Pathogenesis and precision medicine for predicting response in inflammatory bowel disease: advances and future directions, eGastroenterology (2024). DOI: 10.1136/egastro-2023-100006
Provided by
First Hospital of Jilin University
Citation:
Unlocking precision medicine for inflammatory bowel disease (2024, February 5)
retrieved 5 February 2024
from https://medicalxpress.com/news/2024-02-precision-medicine-inflammatory-bowel-disease.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
>>> Read full article>>>
Copyright for syndicated content belongs to the linked Source : Medical Xpress – https://medicalxpress.com/news/2024-02-precision-medicine-inflammatory-bowel-disease.html
