Crisis in Global Health Funding as WHO Leader Sounds the Alarm on Unprecedented Cuts
The Director-General of the World Health Organization (WHO) has issued a grave warning regarding significant reductions in global health funding, characterizing these cuts as potentially disastrous for health systems worldwide. This funding crisis is being recognized as one of the most severe in recent history, threatening advancements made in vital areas such as disease management, vaccination efforts, and maternal and child healthcare. Experts are increasingly worried that these drastic financial limitations could worsen existing health disparities, particularly affecting low-income countries that depend heavily on international aid to maintain their healthcare services.
In light of this troubling trend, it is imperative for major international organizations and governments to reassess their commitments to health financing. The repercussions of inadequate funding may manifest through various channels: a resurgence of preventable diseases, rising mortality rates, and an overall decline in public health standards. Critical sectors identified at risk include:
- Vaccination programs
- Treatment and prevention initiatives for HIV/AIDS
- Primary healthcare services
- Tuberculosis control efforts
This urgent situation calls upon stakeholders within global health to act promptly and collaboratively to restore necessary funding levels. Ensuring that essential health initiatives remain operational is crucial for supporting the world’s most vulnerable populations.
Impact of Funding Cuts on Public Health Initiatives and Global Disease Management
The announcement from the WHO regarding unprecedented reductions in global health financing has sparked serious concerns among public health experts and policymakers alike. These cuts threaten to significantly impede progress against infectious diseases while potentially reversing years of advancements achieved through critical public health initiatives. Affected areas may include:
- Vaccine Distribution: A decrease in funds could hinder efforts aimed at vaccinating at-risk populations against preventable illnesses.
- Disease Surveillance: Limited resources might restrict capabilities needed for monitoring outbreaks like measles or tuberculosis.
- Research & Development: Financial constraints could stall essential research projects required for developing new treatments or vaccines.
- Health Education Programs: Initiatives designed to inform communities about potential health risks may face severe budget cuts, leading to misinformation and increased susceptibility.
The consequences extend beyond immediate public health issues; they pose a threat to global security concerning disease management. An effective response requires coordinated international collaboration—a task complicated by insufficient financial backing. The following implications have been identified as critical:
| Description of Implications | Possible Outcomes |
|---|---|
| Epidemic Resurgence | An increased likelihood of epidemics due to inadequate monitoring capabilities. |
| Inequity Among Nations |
Countries with lower income levels may find it even more challenging to access necessary resources. |
| Erosion of Public Trust |
A decline in trust towards healthcare institutions might occur due to service disruptions caused by budget cuts. |
Recovery Strategies: Recommendations for Sustainable Investment in Global Health Systems
The recent statements from the WHO leader highlight an urgent need for reevaluating how we fund our global healthcare systems. Recognizing shifts within public health landscapes, experts propose several strategies aimed at adapting financial frameworks effectively:
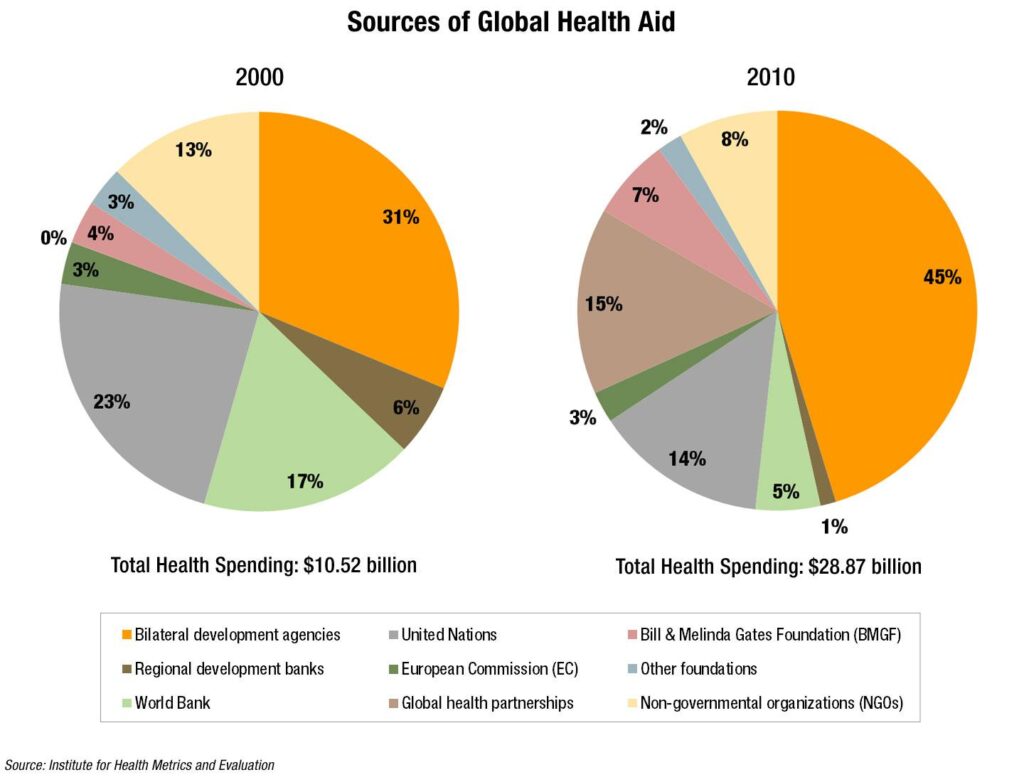
- Diversifying Funding Sources: Exploring alternative revenue streams such as partnerships between private entities & local philanthropic ventures.
- Improving Efficiency: Prioritizing investments into technologies & management systems that can reduce operational costs while enhancing service delivery.
- Data-Driven Resource Allocation: Implementing evidence-based strategies ensures funds are directed toward pressing challenges within healthcare.
Additionally , fostering collaborative alliances among nations can promote shared responsibility towards improving global well-being . Constructive partnership models should focus on:
Type Of Partnership Objective Bilateral Agreements Enhance resilience through resource sharing . Regional Collaborations Facilitate cross-border initiatives & emergency preparedness . Global Coalitions Conclusion The alarming warnings issued by the head official from WHO signify a pivotal moment concerning worldwide investment into our collective wellbeing . As nations confront unprecedented fiscal reductions , potential ramifications loom large—impacting everything ranging from pandemic readiness downwards towards basic services available amongst vulnerable communities . A unified commitment revitalizing budgets dedicated solely towards improving human lives remains paramount if we wish safeguard future generations’ prospects . In navigating turbulent waters ahead , recognizing investments made today aren’t merely economic necessities but moral obligations protecting those who need it most becomes increasingly vital ; thus shaping tomorrow’s landscape rests firmly upon actions taken now!
- Improving Efficiency: Prioritizing investments into technologies & management systems that can reduce operational costs while enhancing service delivery.