Glut1 deficiency syndrome, a neurological disease caused by a genetic mutation leading to insufficient glucose for the brain, can cause seizures, abnormal movement, and developmental delays. Scientists have developed a blood test called METAglut1, which can diagnose the disease quickly, bypassing the need for an invasive lumbar puncture, with a sensitivity of about 80% and specificity of more than 99%.
Glut1 deficiency syndrome is a relatively obscure neurological condition that remains unknown to the medical community, despite its serious debilitating effects. The disorder results from a mutation in the SLC2A1 gene, leading to an impaired glucose transporter, GLUT1, in affected individuals. Since this transporter plays a critical role in facilitating glucose uptake into glial cells, its malfunction leaves the brain with insufficient sugar necessary for optimal functionality. As a result, patients experience seizures, episodes of unusual movements, and developmental delays.
However, the adverse symptoms can be mitigated by managing the metabolic anomaly causing the disease by adopting a high-fat ketogenic diet. In addition, promising new therapeutic molecules designed to compensate for the poor supply of glucose to brain cells are currently being evaluated.
“Patients who are not diagnosed suffer a regrettable loss of opportunity. They could be treated, says Professor Fanny Mochel, principal investigator of the study. There is an urgent need to identify them better since many are missing or diagnosed too late.”
The incidence of Glut1 deficiency syndrome is estimated to be 1 in 24,000 in the general population. This figure is probably underestimated, as it only considers epileptic patients and not those with isolated, non-specific symptoms such as learning disabilities or abnormal movements. The diagnosis is even more challenging to make because it was previously based on a lumbar puncture supplemented by genetic tests.
“This invasive, often lengthy, and expensive procedure significantly limits access to care, adds the researcher. Hence the interest in looking for a blood biomarker to enable a rapid diagnosis of Glut1 deficiency syndrome.”
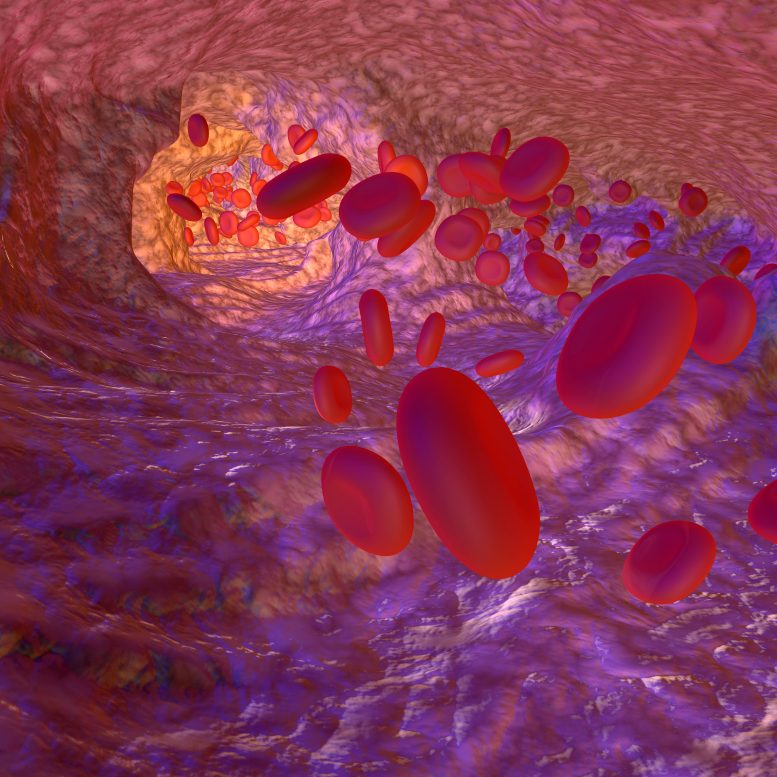
Red blood cells lined with clues
Indeed, the GLUT1 transporter is not only abundant in endothelial and glial cells of the brain: it also binds to the surface of erythrocytes, the red blood cells. The diagnostic test designed by the Paris-based medtech METAFORA biosystems makes it possible to quantify GLUT1 on their surface by flow cytometry, a technique routinely used in analysis laboratories. A simple blood sample is required to perform the test without the need to take a fasting patient. The result is available in 48 to 72 hours.
To validate the new test – METAglut1 – teams from AP-HP and 33 French clinical investigation centers, under the direction of Professor Fanny Mochel, recruited 549 patients in a prospective cohort – that is to say, people in whom the disease was suspected – and 87 patients from a retrospective cohort, already diagnosed. The goal? To compare the efficacy and accuracy of METAglut1 with the reference diagnostic test requiring cerebrospinal fluid sampling and genetic analysis.
The researchers’ results indicate that METAglut1 has a sensitivity of about 80%, a specificity of more than 99%, and a high predictive value, a performance comparable to the reference test. “These data allow us to validate the benefit of the test formally, says Professor Fanny Mochel. It will make it possible to look for Glut1 deficiency syndrome in many patients simply and quickly. In the event of a positive result, treatment can be started immediately, significantly improving the prognosis, especially for children in the midst of brain development.”
Therefore, the study’s authors recommend that the test be performed in all children from 3 months of age and adults with intellectual disability, neurodevelopmental disorders, abnormal movements, or epilepsy – especially if it is drug-resistant and if a ketogenic diet alleviates the seizures. Indeed, if used at an early symptomatic stage, METAglut1 can immediately identify 80% of patients with Glut1 deficiency syndrome. For this reason, French National Authority for Health recommends its reimbursement, which paves the way for its adoption in Europe and the US.
Reference: “Prospective Multicenter Validation of a Simple Blood Test for the Diagnosis of Glut1 Deficiency Syndrome” by Fanny Mochel, Domitille Gras, Marie-Pierre Luton, Manon Nizou, Donatella Giovannini, Caroline Delattre, Mélodie Aubart, Magalie Barth, Anne De Saint-Martin, Diane Doummar, Nouha Essid, Alexa Garros, Caroline Hachon Le Camus, Celia Hoebeke, Sylvie Nguyen The Tich, Maximilien Perivier, Serge Rivera, Anne Rolland, Agathe Roubertie, Catherine Sarret, Caroline Sevin, Dorothee Ville,Marc Sitbon, Jean-Marc Costa, Roser Pons, Angels Garcia-Cazorla, Sandrine Vuillaumier, Vincent Petit, Odile Boespflug-Tanguy and Darryl C. De Vivo, for the MetaGlut1 Study Group, 19 April 2023, Neurology.
DOI: 10.1212/WNL.0000000000207296
>>> Read full article>>>
Copyright for syndicated content belongs to the linked Source : SciTechDaily – https://scitechdaily.com/simple-blood-test-can-now-diagnose-de-vivo-disease/