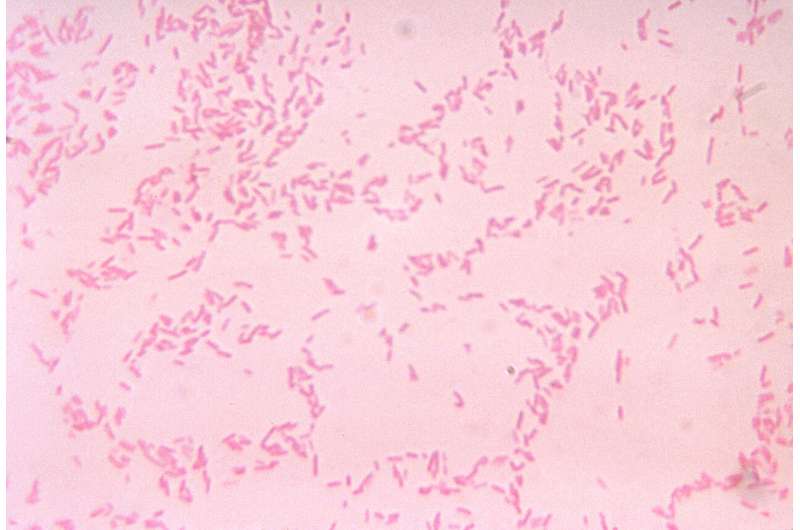
B. fragilis is a commensal bacteria that normally lives in the human gastrointestinal tract. It can become pathogenic due to disruption of the normal intestinal mucosa through trauma or surgery. Credit: Centers for Disease Control/V.R. Dowell Jr.
Antibiotic resistance is a significant and growing medical problem worldwide. Researchers at the Marine Biological Laboratory (MBL) and collaborators have found a novel genetic arrangement that may help a common bacterium in the human gut, Bacteroides fragilis, protect itself from tetracycline, a widely used antibiotic.
While these findings will not lead directly to new ways of combating tetracycline-resistant bacteria, the researchers have discovered previously unseen genetic arrangements that confer antibiotic resistance. Such understanding might help in developing new ways to limit the spread of antibiotic resistance genes, through genetic manipulation or other means.
The findings were reported in the journal mBio by MBL scientists Joseph Vineis, Mitchell Sogin and Blair Paul, along with colleagues from MBL, Argonne National Laboratory, and the University of Chicago.
The bacteria they studied, Bacteroides fragilis, was recovered from a patient with ulcerative colitis, where it was found to be abundant during periods of inflammation. The team had a large set of samples to analyze from patients with inflammatory bowel disease that had been surgically treated to alleviate the inflammation.
These samples were studied at MBL using shotgun metagenomics, which produces sequences for all the genetic material in an entire community of microbial cells. It also facilitates cultivation of bacterial strains from the community, providing the data required to observe the activity of the tetracycline-resistance genes while growing in the presence of tetracycline. (At the time they started this work, Vineis says, “to be able to reconstruct genomes from metagenomic data was just getting started in the field. It was a novel approach, but now it’s common.”)
“When we looked at the data,” Vineis says, “there was a very strong signal” showing high numbers of copies of particular regions of the bacterial genomes. One of these regions, encompassing many genes, “was very abundant” in the sample, and later they were able to determine “that this particular high-copy region contained tetracycline resistance… So we kept digging.”
These high-copy sections of the genome contained DNA fragments that can move around in the genome or even jump into a different genome. Called transposons, these mobile genetic elements are “important ways for bacteria to develop adaptations to the environment without having to reinvent them themselves completely,” Vineis says. And in the human intestines, where vast numbers of species of gut bacteria are constantly in close proximity, “the potential for exchange is really high,” he says, and the rate increases when there is inflammation.
Such exchange of genetic material between different species is called horizontal transfer. Blair Paul, an assistant scientist at MBL, says that “we think these transposons are actually a key vehicle for horizontal gene transfer.”
In this case, the bacteria apparently sense when there is tetracycline in the environment and begin “a whole cascade” of production of a transposon containing the resistance gene, Vineis says.
The part of the transposon containing the resistance gene, they found, occurred in two different forms within the same genome: Sometimes it is in its normal linear form, and sometimes rolled into a circle. Both forms occur at once in the Bacteroides fragilis genome, but the linear form contains a unique genomic insert in the region of DNA that encodes the machinery for mobilization into other cells.
“This hasn’t been seen before, to our knowledge,” Paul says, “this particular type of transposon having a subregion amplified. And it’s occurring in bacteria that coincide with inflammation.”
The increased expression of this group of genes is potentially associated with the success of Bacteroides fragilis during inflammation, although the connection is not yet proven and requires further research. But Paul says the findings “raise new questions about the role of gene transfer in human health, but also in terms of just how these transposons are controlled and how they may be changing evolutionarily over time.”
“This finding is not going to change our understanding about the world of antibiotic resistance, but it’s a novel kind of mechanism that at least we can start looking for,” Vineis says. “There’s a lot of offense and defense happening within the microbial world that we’re not even fully aware of.”
More information:
A novel conjugative transposon carrying an autonomously amplified plasmid, mBio (2024). DOI: 10.1128/mbio.02787 , journals.asm.org/doi/10.1128/mbio.02787-23
Journal information:
mBio
Citation:
Team finds novel vehicle for antibiotic resistance (2024, March 1)
retrieved 2 March 2024
from https://phys.org/news/2024-03-team-vehicle-antibiotic-resistance.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
>>> Read full article>>>
Copyright for syndicated content belongs to the linked Source : Phys.org – https://phys.org/news/2024-03-team-vehicle-antibiotic-resistance.html










