In the intricate dance of human metabolism, the balance between hunger and satiety plays a crucial role in regulating our dietary choices and overall health. Recent groundbreaking research has illuminated a fascinating interplay between neurobiology and our craving for sugar, revealing that thalamic opioids released from pro-opiomelanocortin (POMC) satiety neurons may be a key player in this complex equation. This unexpected connection challenges conventional wisdom about hunger signals and offers a fresh lens through which to examine the mechanisms underlying our sweet cravings. As we delve into the findings of this study, we will explore how these neural pathways not only influence our appetite for sugar but potentially reshape our understanding of dietary behaviors and their implications for metabolic health.
Exploring the Role of Thalamic Opioids in Sugar Cravings
The intricate relationship between thalamic opioids and sugar cravings unveils a fascinating aspect of our neurobiology that goes beyond mere dietary choices. Research indicates that the activation of proopiomelanocortin (POMC) neurons in the hypothalamus plays a critical role in regulating satiety. However, new findings suggest that thalamic opioids derived from these neurons may actually trigger an appetite for sugary substances, showcasing a dual role not previously understood. This paradox highlights the complexities of our reward systems and hunger signals.
Key mechanisms at play include:
- Neuronal Activation: Specific opioids in the thalamus interact with reward pathways, influencing hedonic motivations towards sugar.
- Hormonal Responses: The release of thalamic opioid peptides could potentially alter insulin sensitivity, further complicating our cravings.
- Behavioral Outcomes: Individuals exposed to certain stimuli may exhibit pronounced cravings driven by thalamic opioid activity.
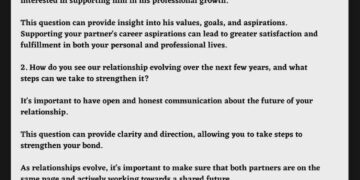
A closer examination of this phenomenon could provide essential insights into diet-related behavioral patterns. The following table summarizes the interactions between thalamic opioids and sugar consumption:
| Interaction | Effect on Cravings |
|---|---|
| Thalamic Opioid Release | Increases sugar-seeking behavior |
| Enhanced Reward Processing | Augments pleasure derived from sweet foods |
| POMC Neuron Activation | Conflicting signals regarding satiety |
Understanding the dual nature of thalamic opioids opens up new avenues for addressing sugar addiction and obesity. This nuanced perspective not only contributes to our comprehension of dietary choices but also paves the way for innovative treatments targeting opioid pathways in the brain. As research progresses, further insights may emerge, guiding interventions tailored to manage sugar cravings and promote healthier eating behaviors.

The Connection Between POMC Neurons and Appetite Regulation
New research reveals the intricate relationship between POMC (Pro-opiomelanocortin) neurons and the regulation of appetite, particularly in relation to sugar cravings. These specialized neurons, located in the hypothalamus, play a crucial role in signaling satiety. When activated, POMC neurons release key peptides that promote feelings of fullness and reduce hunger. This regulatory pathway suggests that the brain’s biochemical environment directly influences our food preferences and choices, especially when it comes to sugars.
Interestingly, the presence of thalamic opioids derived from these POMC neurons introduces a fascinating twist in the appetite control narrative. This connection highlights that while POMC neurons work to curb appetite, they also possess the intriguing ability to switch on the desire for sugar. This dual functionality may be attributed to the brain’s complex reward system, driving individuals to seek out sweeteners during times of stress or fatigue, despite the body’s signals of satiety.
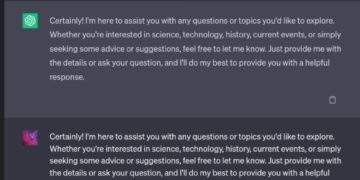
To illustrate the impact of POMC neurons on appetite regulation, consider the following table showcasing the key factors involved in this process:
| Factor | Effect on Appetite |
|---|---|
| POMC Neurons | Promote satiety |
| Thalamic Opioids | Enhance sugar craving |
| Satiety Signals | Inhibit hunger |
| Stress Levels | Increase sugar desire |
This dynamic interaction raises important questions about dietary behaviors and potential therapeutic targets for obesity and eating disorders. As scientists continue to unravel the complexities of neural pathways and their effects on our food choices, a deeper understanding of these mechanisms could pave the way for innovative approaches to appetite regulation and the management of sugar consumption.
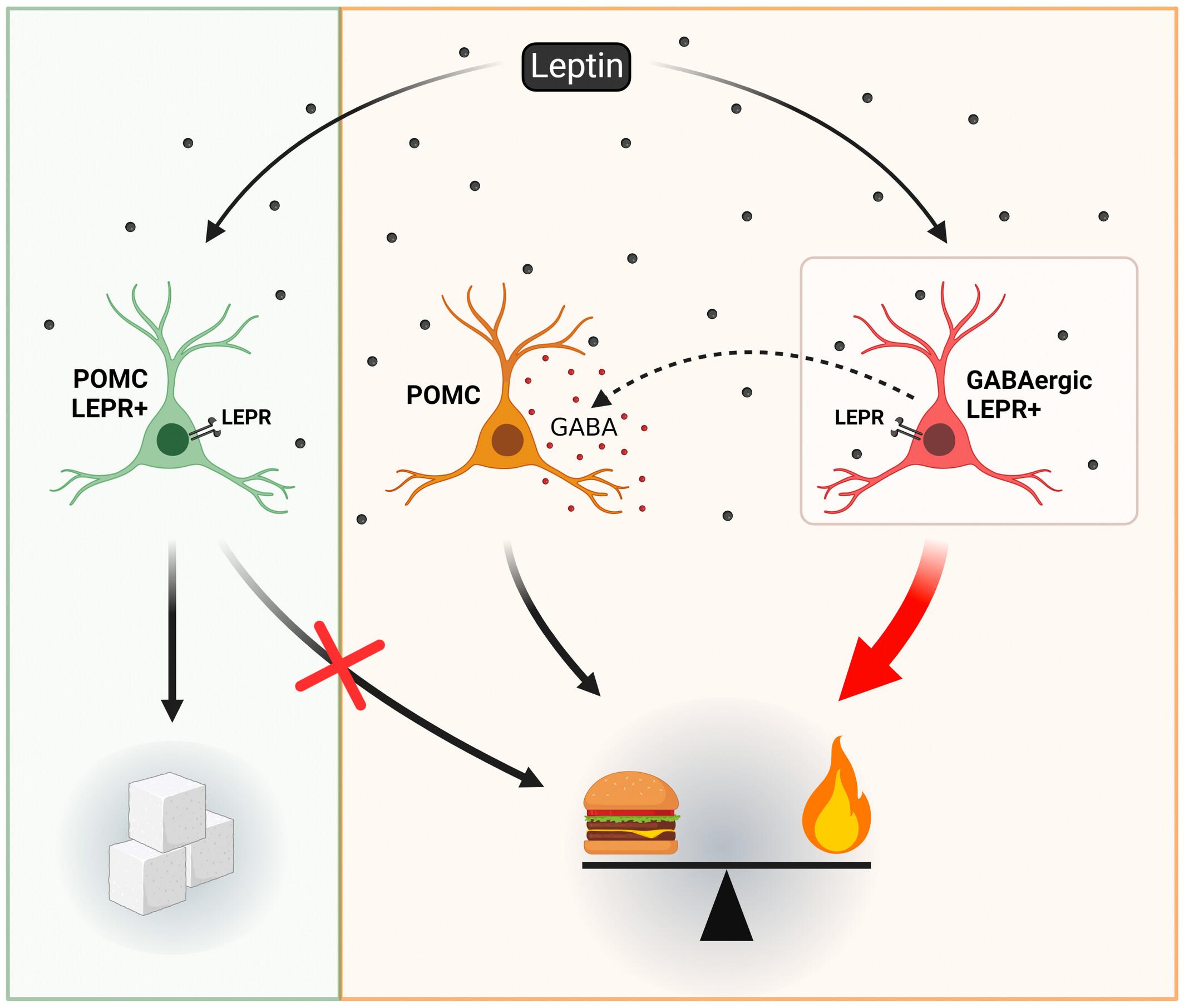
Implications for Understanding Obesity and Sugar Consumption
The recent findings regarding thalamic opioids produced by POMC satiety neurons open a new frontier in understanding how our brains regulate sugar consumption. These neurons play a crucial role in the delicate balance of energy homeostasis, yet the discovery that they can switch on sugar appetite suggests a complex relationship between satiety and cravings. This unearths the potential that what we perceive as hunger for sugar might not solely be driven by energy deficiency, but rather by neural pathways that respond to sugar in a particular way. A deeper investigation into this mechanism could reshape current strategies for addressing dietary habits.
Moreover, this revelation raises significant questions about the broader implications of sugar intake on overall health. The identification of thalamic opioids emphasizes the interplay between craving mechanisms and hormonal regulation. Understanding these networks could lead to innovative approaches to combat obesity and curtail excessive sugar consumption. Numerous factors may influence this relationship, including:
- Genetic predisposition – Individual variations in opioid receptor sensitivity.
- Environmental influences – Accessibility to sugary foods and marketing strategies targeting sugar consumption.
- Psychological factors – Stress and emotional eating linked to sweet cravings.
As researchers continue to explore the functionality of POMC neurons and their opioid output, it becomes increasingly clear that sugar addiction may have more profound biological underpinnings than previously recognized. This understanding could inform public health initiatives, dietary guidelines, and therapeutic interventions aimed at reducing obesity rates. Ultimately, there is a growing need to prioritize the exploration of biochemical drivers behind dietary choices, as these insights will be pivotal in shaping effective solutions to one of the most pressing health challenges of our time.
Strategies to Target Thalamic Pathways for Appetite Control
Targeting thalamic pathways presents a promising avenue for appetite control, especially in the context of understanding the role of opioids derived from pro-opiomelanocortin (POMC) neurons. Through the modulation of these pathways, researchers can potentially influence the neurobiological mechanisms responsible for cravings and satiety. By investigating the intricate connections between the thalamus and appetite regulation, we can develop strategies to promote healthier eating behaviors and combat obesity.
Key strategies may include:
- Pharmacological Interventions: Developing medications that specifically target thalamic opioid receptors could help regulate sugar cravings and contribute to better appetite management.
- Neurostimulation Techniques: Utilizing methods like transcranial magnetic stimulation (TMS) to influence thalamic activity may offer a non-invasive way to modulate appetite signals.
- Behavioral Approaches: Integrating behavioral therapy with a focus on understanding and reshaping the neural pathways activated during sugar cravings could enhance the effectiveness of traditional dietary interventions.
In addition to these strategies, ongoing research into the thalamic circuitry linked to reward and hunger can inform our approach to appetite control. By mapping out the specific neural pathways involved, scientists can better understand the bidirectional relationship between satiety signals and the drive for sugary foods. A deeper understanding of this neurochemical landscape opens the door to innovative treatments tailored to disrupt pathological eating behaviors and foster a balanced approach to nourishment.

Closing Remarks
the intricate dance between thalamic opioids and the body’s hunger cues opens a fascinating window into the regulation of appetite, particularly for sugar. As the findings from recent research underscore, the role of POMC satiety neurons extends far beyond merely signaling fullness; they also hold the key to understanding the cravings that can drive our dietary choices. The revelation that thalamic opioids can modulate sugar appetite not only enhances our comprehension of metabolic processes but also poses important questions for future research into the complex interplay of nutrition, pleasure, and satiety. As we continue to unravel these neural pathways, we yet again find ourselves at the crossroads of behavioral science and the quest for healthier eating habits. What other secrets might the brain hold about our appetites? The journey to uncover them has only just begun.